Navigating the Network: A Comprehensive Guide to the Cranial Nerves
Related Articles: Navigating the Network: A Comprehensive Guide to the Cranial Nerves
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Navigating the Network: A Comprehensive Guide to the Cranial Nerves. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating the Network: A Comprehensive Guide to the Cranial Nerves
The human nervous system, a complex and intricate network, is responsible for everything from basic reflexes to conscious thought. Within this network, a specialized set of nerves, known as the cranial nerves, emerge directly from the brain and connect to various parts of the head, neck, and even the torso. These twelve pairs of nerves, each with its unique function, play a vital role in controlling sensory input, motor output, and autonomic functions, making them essential for a wide range of bodily processes.
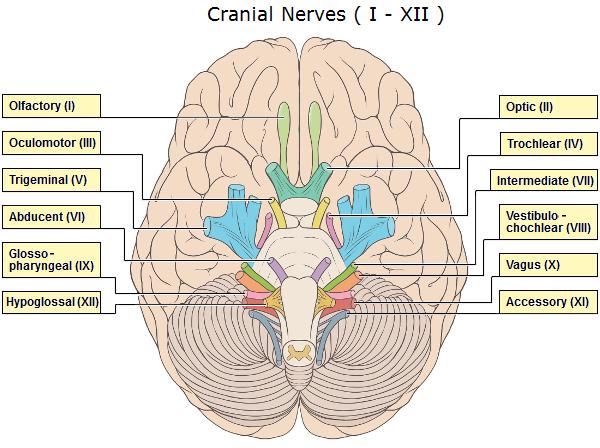
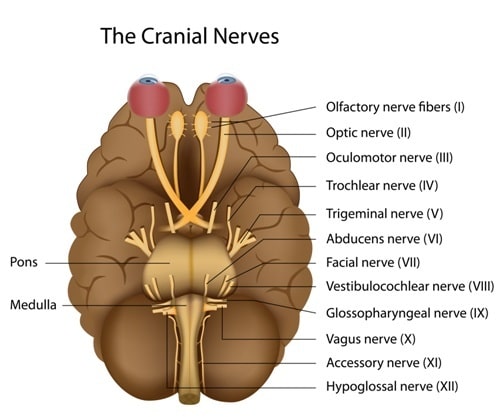
Understanding the Cranial Nerve Map
A visual representation of the cranial nerves, often called a "map," is an invaluable tool for understanding their organization and function. This map typically depicts the twelve cranial nerves, numbered from I to XII, with their corresponding names, origins, pathways, and target organs. Each nerve is assigned a Roman numeral based on its anatomical location, with the olfactory nerve (I) being the most anterior and the hypoglossal nerve (XII) the most posterior.
A Detailed Look at the Cranial Nerves
Let’s explore each of the twelve cranial nerves in detail, understanding their functions and clinical significance:
I. Olfactory Nerve:
- Function: Responsible for the sense of smell.
- Pathway: Originates in the olfactory epithelium of the nasal cavity and travels to the olfactory bulb in the brain.
- Clinical Significance: Damage to this nerve can result in anosmia, the inability to smell.
II. Optic Nerve:
- Function: Carries visual information from the eye to the brain.
- Pathway: Originates in the retina of the eye and travels to the optic chiasm, where fibers from each eye cross over, and then to the thalamus and visual cortex.
- Clinical Significance: Damage to this nerve can lead to vision loss, ranging from partial blindness to complete blindness, depending on the extent of the damage.
III. Oculomotor Nerve:
- Function: Controls four of the six extraocular muscles responsible for eye movement, as well as the pupillary sphincter muscle (constricting the pupil) and the ciliary muscle (adjusting lens shape for focusing).
- Pathway: Originates in the midbrain and travels to the superior, inferior, and medial rectus muscles, the inferior oblique muscle, the pupillary sphincter, and the ciliary muscle.
- Clinical Significance: Damage to this nerve can result in diplopia (double vision), ptosis (drooping eyelid), and pupillary dilation.
IV. Trochlear Nerve:
- Function: Controls the superior oblique muscle, responsible for downward and outward eye movement.
- Pathway: Originates in the midbrain and travels to the superior oblique muscle.
- Clinical Significance: Damage to this nerve can lead to diplopia, particularly when looking downward.
V. Trigeminal Nerve:
- Function: The largest cranial nerve, responsible for sensory innervation of the face, scalp, and teeth, as well as motor innervation of the muscles of mastication (chewing).
- Pathway: Has three branches: the ophthalmic nerve (sensory, supplying the forehead, eye, and upper face), the maxillary nerve (sensory, supplying the cheek, upper teeth, and palate), and the mandibular nerve (mixed, supplying the lower teeth, jaw, and muscles of mastication).
- Clinical Significance: Damage to this nerve can cause pain, numbness, or weakness in the face, as well as difficulty chewing.
VI. Abducens Nerve:
- Function: Controls the lateral rectus muscle, responsible for outward eye movement.
- Pathway: Originates in the pons and travels to the lateral rectus muscle.
- Clinical Significance: Damage to this nerve can lead to diplopia, particularly when looking to the side.
VII. Facial Nerve:
- Function: Controls facial expressions, taste sensation from the anterior two-thirds of the tongue, and salivary gland secretions.
- Pathway: Originates in the pons and travels to the muscles of facial expression, the submandibular and sublingual salivary glands, and the taste buds of the anterior tongue.
- Clinical Significance: Damage to this nerve can cause facial paralysis, loss of taste, and dry mouth.
VIII. Vestibulocochlear Nerve:
- Function: Responsible for hearing and balance.
- Pathway: Has two branches: the cochlear nerve (carries auditory information from the cochlea to the brain) and the vestibular nerve (carries balance information from the inner ear to the brain).
- Clinical Significance: Damage to this nerve can lead to hearing loss, tinnitus (ringing in the ears), dizziness, and loss of balance.
IX. Glossopharyngeal Nerve:
- Function: Controls swallowing, taste sensation from the posterior third of the tongue, and salivary gland secretions.
- Pathway: Originates in the medulla oblongata and travels to the stylopharyngeus muscle (swallowing), the parotid salivary gland, and the taste buds of the posterior tongue.
- Clinical Significance: Damage to this nerve can cause difficulty swallowing, loss of taste, and dry mouth.
X. Vagus Nerve:
- Function: The longest cranial nerve, responsible for a wide range of functions, including heart rate, digestion, and vocalization.
- Pathway: Originates in the medulla oblongata and travels to the heart, lungs, digestive system, and larynx.
- Clinical Significance: Damage to this nerve can cause a variety of symptoms, including heart rate irregularities, difficulty swallowing, hoarseness, and gastrointestinal problems.
XI. Accessory Nerve:
- Function: Controls the sternocleidomastoid and trapezius muscles, responsible for head movement and shoulder elevation.
- Pathway: Originates in the medulla oblongata and spinal cord and travels to the sternocleidomastoid and trapezius muscles.
- Clinical Significance: Damage to this nerve can cause weakness or paralysis of the head and shoulder muscles.
XII. Hypoglossal Nerve:
- Function: Controls tongue movement.
- Pathway: Originates in the medulla oblongata and travels to the muscles of the tongue.
- Clinical Significance: Damage to this nerve can cause difficulty speaking, chewing, and swallowing.
Clinical Importance of the Cranial Nerve Map
The map of cranial nerves is a fundamental tool for healthcare professionals, particularly neurologists and otolaryngologists. It allows them to:
- Diagnose neurological disorders: By assessing the function of individual cranial nerves, doctors can identify specific areas of the nervous system that are affected.
- Locate the site of a lesion: The pattern of cranial nerve dysfunction can help pinpoint the location of a tumor, stroke, or other neurological injury.
- Monitor treatment progress: Observing changes in cranial nerve function can help doctors track the effectiveness of treatment for neurological disorders.
- Plan surgical interventions: Understanding the anatomy and function of cranial nerves is crucial for surgeons performing procedures involving the head and neck.
FAQs About the Cranial Nerves
1. What are the symptoms of a cranial nerve disorder?
Symptoms of a cranial nerve disorder vary depending on the affected nerve and the extent of the damage. Common symptoms include:
- Sensory loss: Numbness, tingling, or loss of sensation in the face, head, or tongue.
- Motor weakness: Difficulty moving the eyes, face, tongue, or neck.
- Balance problems: Dizziness, vertigo, or difficulty walking.
- Hearing loss: Difficulty hearing or tinnitus.
- Vision loss: Partial or complete blindness.
- Swallowing difficulties: Dysphagia.
- Speech problems: Dysarthria.
- Facial paralysis: Bell’s palsy.
2. What causes cranial nerve disorders?
Cranial nerve disorders can be caused by a variety of factors, including:
- Trauma: Head injury or surgery.
- Tumors: Benign or malignant growths.
- Stroke: Blood clot or blockage in the brain.
- Infections: Meningitis, encephalitis.
- Autoimmune disorders: Multiple sclerosis, Guillain-Barré syndrome.
- Nutritional deficiencies: Vitamin B12 deficiency.
- Toxic exposures: Heavy metals, pesticides.
3. How are cranial nerve disorders diagnosed?
Cranial nerve disorders are diagnosed through a thorough medical history, physical examination, and specialized tests, such as:
- Neurological examination: Assessment of cranial nerve function, reflexes, and sensory perception.
- Imaging studies: MRI or CT scans to visualize the brain and surrounding structures.
- Electrophysiological tests: Electroencephalography (EEG) to measure brain activity, electromyography (EMG) to measure muscle activity, and electroneurography (ENG) to measure nerve conduction velocity.
4. What is the treatment for cranial nerve disorders?
Treatment for cranial nerve disorders depends on the underlying cause and the severity of symptoms. Options may include:
- Medication: Anti-inflammatory drugs, antiviral medications, or corticosteroids.
- Surgery: To remove tumors, relieve pressure, or repair damaged nerves.
- Physical therapy: To improve muscle strength and coordination.
- Speech therapy: To improve speech and swallowing.
- Occupational therapy: To improve daily living skills.
Tips for Maintaining Cranial Nerve Health
While there’s no guaranteed way to prevent all cranial nerve disorders, certain lifestyle choices can promote overall neurological health:
- Maintain a healthy diet: Consume a balanced diet rich in fruits, vegetables, and whole grains.
- Exercise regularly: Physical activity improves blood flow to the brain and supports overall health.
- Manage stress: Chronic stress can negatively impact the nervous system. Engage in stress-reducing activities like yoga, meditation, or spending time in nature.
- Avoid smoking and excessive alcohol consumption: These substances can damage the nervous system.
- Get regular checkups: Early detection and treatment are crucial for managing neurological disorders.
Conclusion
The map of cranial nerves serves as a valuable roadmap for understanding the complex network of nerves that control our sensory experiences, motor functions, and vital bodily processes. By appreciating the intricate workings of these twelve pairs of nerves, we gain a deeper understanding of the human nervous system and its role in maintaining our health and well-being. Understanding the functions and potential issues associated with each cranial nerve empowers individuals to better understand their own health and seek appropriate medical attention when necessary.
Closure
Thus, we hope this article has provided valuable insights into Navigating the Network: A Comprehensive Guide to the Cranial Nerves. We appreciate your attention to our article. See you in our next article!
